Watch Evaluate Better: A Guide to Using ACGME Milestones
Clinical Competency Committee (CCC) meetings are a common program requirement where you audit your own evaluation process. Milestones spring reporting takes place through June, and these competency-based markers can be a powerful assessment tool for both individual residents and fellows, as well as your program curriculum as a whole.
As a relatively new assessment tool, ACGME Milestones have created a paradigm shift in how we evaluate. You may find yourself questioning whether or not your program is maximizing its potential. How do ACGME Milestones fit into other assessment tools? What role does the CCC play in ACGME Milestones? And how can ACGME Milestones be leveraged to help strengthen individual skills and overall curriculum development?
MedHub hosted a webinar in April of 2021, “Evaluate Better: A Guide to Using Milestones”, presented by Kate McDaniel, Ph.D., MSW, to help Program Directors, CCC members, and GME program faculty better understand the role and purpose of ACGME Milestones so you can — as the name suggests — evaluate better. Dr. McDaniel is an Assistant Professor and the GME Educator in charge of Faculty Development at Duke University Hospital and Health System in the department of Neurosurgery, and spent five years as the GME Education Specialist at St. Louis University. Below are some key takeaways from Dr. McDaniel’s presentation.
How do ACGME Milestones fit within the context of GME assessment?
No single tool can determine readiness for independent practice. ACGME Milestones are not meant to be stand-alone evaluation forms or direct assessment tools, but rather to provide a framework for residency programs to move trainees toward competent, unsupervised practice. These Milestones create a shared language for residents and fa
culty, describing the learning trajectory for trainees within the core competencies.
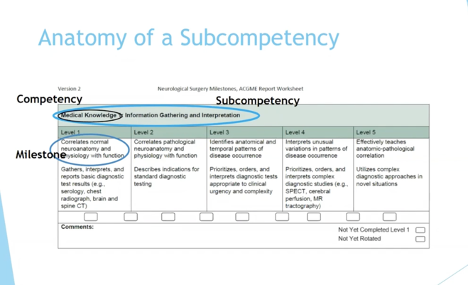
ACGME Milestones were first introduced into the graduate medical education landscape in 2013. What is unique about them is that they are organized by behavioral anchors, which tie to sub-competencies within the six ACGME core competencies.
Using multiple assessment tools — formative and summative — gives a clearer picture of how learners are progressing. From end-of-rotation evaluations, to direct observation and case logs, there are numerous assessment tools available, and all should be considered when determining ACGME Milestone markers.
Before Milestones, there was a wide variance on what deemed a trainee “competent.” Milestones help to standardize competency in a new way that’s based on actual behavior.
How the Clinical Competency Committee (CCC) informs ACGME Milestone ratings
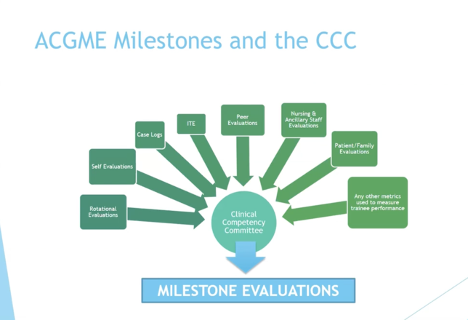
All ACGME-accredited programs are required to have a Clinical Competency Committee (CCC). Its members are appointed by the Program Director and must include at least three faculty members, who meet a minimum of two times per year to discuss resident performance. Specific details about CCC composition expectations are found in the Program Requirements (both in the Common Program Requirements for Residencies, Fellowships, One-Year Fellowships, and Post-Doctoral Education Programs, and also in the specialty- and subspecialty-specific Program Requirements).
The CCC plays a critical role in ACGME Milestone reporting. It is the funnel all resident assessments go through before determining a rating for each sub-competency within your specialty’s Milestones. Committee members review all data — rotational evaluations, peer evaluations, case logs, etc. — and use it to determine a rating for each sub-competency. These Milestone assessments are provided to the Program Director who then reviews and reports them to the ACGME.
ACGME Milestones are not a shortcut. Dr. McDaniel stresses that it can be tempting to use the Milestone rubric in the place of other assessment tools, but that doing so diminishes the value of Milestones, which are meant to help distill a much broader picture.
How to leverage ACGME Milestones to assist struggling residents and perform a curricular assessment
ACGME Milestone evaluation gives you an opportunity to look at both individual trainees, as well as the curriculum as a whole.
You can identify struggling residents sooner and help them create a more explicit improvement plan. For example, if a resident was at level 2, but they are expected to be at level 3, you can create an actionable plan with steps to take to get there. This can be particularly helpful in sub-competencies that are less clinical; “harmonized” Milestones such as Interpersonal Communication Skills.
You may find, when assessing Milestones, that you have some gaps in your teaching, your assessments, or both. If you map how each sub-competency is taught and the tool(s) that are used to evaluate performance, you could discover that you don’t have adequate data to evaluate an ACGME Milestone and can adjust your curriculum or evaluations accordingly.
Watch the Full Webinar
Complete the form below to access the full webinar, Evaluate Better: A Guide to Using Milestones.